WCH Medical Billing Franchise: proven model, software, training, and step-by-step support to operate and scale.
Business Services, Healthcare & Senior CareAbout WCH Service Bureau
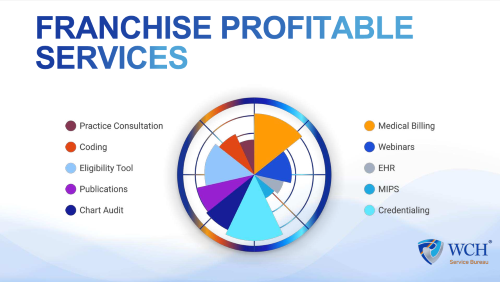
With over 20 years in U.S. healthcare administration, WCH helps entrepreneurs build sustainable medical billing operations. Our franchise offers a structured, fully supported path into revenue cycle management—combining a proven operating model, proprietary software, payer-aligned workflows, and step-by-step training from industry experts. From defining your specialty focus and pricing to implementing HIPAA-compliant procedures and performance standards, we provide the clarity and tools you need to serve physician clients with confidence while maintaining a clean, compliant operation.
Your launch is guided by a hands-on, milestone-based program. You’ll receive a complete go-to-market toolkit, credentialing and payer enrollment playbooks, coding quality assurance processes, denial-prevention protocols, and ongoing audits. The model is service-based, with lean overhead and recurring revenue streams across billing, coding, and credentialing—enabling steady, client-by-client growth, from your first prospect to your first clean claim and beyond.
2019 (7 years)
-
-
Franchise Fees
$45,000
7.0% - 10.0%
Gross Revenues
5.0%
Marketing Budget
Why WCH Service Bureau?
- 20+ Years of Expertise: We turn decades of U.S. healthcare administration into a clear, supported path to launch your own medical billing firm.
- Proven System: Proprietary software and step-by-step workflows for coding, claims, denials, A/R, and compliance.
- Fast Launch: 30/60/90-day plan with positioning, pricing, prospecting tools, and onboarding checklists to get you revenue-ready.
- Multiple Revenue Streams: Billing, coding QA, and credentialing/enrollment for recurring income and stronger client retention.
- Hands-On Training: Structured onboarding, role-specific paths and audits to ensure steady progress.
- Built-In Compliance: HIPAA-aligned processes, denial-prevention protocols, and updates as payer rules evolve.
- Lean, Scalable Model: Low overhead, small team structure, and recurring revenue that grows client by client.
- Ongoing Support: Guidance and resources to keep you moving forward..
From your first prospect to your first clean claim—and every client after—WCH gives you the tools and support to scale with confidence.
Ideal Candidate
- You’re a coachable owner-operator who enjoys selling, managing processes, and leading a small team. You value clarity, compliance, and steady execution.
- Consultative B2B seller. Comfortable meeting physicians and practice managers, running discovery, scoping needs, and presenting proposals with a consistent outreach cadence.
- Process-driven operator. Follows SOPs, documents work, manages checklists, and maintains HIPAA-aligned discipline and accuracy.
- Metrics-minded. Tracks net collections, denial rate, and days in A/R; works from dashboards; uses data to coach the team and improve results.
- Relationship builder. Trustworthy, patient, service-oriented; retains clients through proactive communication and clear reporting.
- Team leader. Able to hire, train, and manage billers/credentialing specialists; sets standards and performs quality reviews.
- Tech-comfortable. Uses CRM, billing software/EDI, and spreadsheets; learns new tools quickly.
- Organized and resilient. Manages pipeline and production in parallel; meets deadlines and follows through.
- Engaged learner. Participates in WCH training, office hours, audits, and executes the 30/60/90 plan.
- Backgrounds that translate well: medical office/practice management, healthcare administration, RCM/billing, payer/insurance operations, accounting/finance, pharmaceutical or med-device sales, B2B services, and operations/project management. Clinical professionals transitioning to business leadership also fit. You won’t be coding or providing clinical care—you’ll run a service business with disciplined operations and client-facing leadership.
$45,000 - $75,000
$45,000
$100,000